Ankylosing Spondylitis (AS) is a chronic inflammatory disease of unknown etiology characterized by prominent inflammation of the spinal joints and adjacent structures. If left untreated, this inflammation can lead to progressive fusion of the spine, chronic back pain, and disability. The joints of the arms and legs are less affected, although the hips and shoulders may become involved in up to one third of cases. Also, inflammation of other parts of the body, such as the eyes, the GI tract, skin, lungs, and heart, may occur.
Males appear to be affected more than females. The average age of onset ranges from adolescence to age 25 and peaks around 28 years. Approximately 15% of adult American and European cases have been found to have a childhood onset.
There is a strong genetic component to the development of AS, with the HLA-B27 gene associated with most cases. A positive family history of AS can be found in 15% to 20% of cases.
In recent years, there have been significant advances in our understanding of AS. We now know that it exists within a spectrum of diseases called spondyloarthritis. Other diseases often included in this category are psoriatic arthritis, reactive arthritis, inflammatory bowel disease, and uveitis.
Symptoms
In most patients, AS can lead to progressive back stiffness and spinal restriction with intermittent exacerbations. Characteristically, the back pain in AS presents as prominent stiffness and pain in the morning or following other periods of rest (gel phenomenon) that improve with exercise and movement. Back pain often forces the individual out of bed at night and is unrelieved by lying down. These symptoms typically develop slowly over months and years. Patients often cannot date when symptoms first began, or precisely localize the areas affected.
The earliest abnormality seen is usually tenderness in the sacroiliac joints, which connect the lower spine to the pelvis.
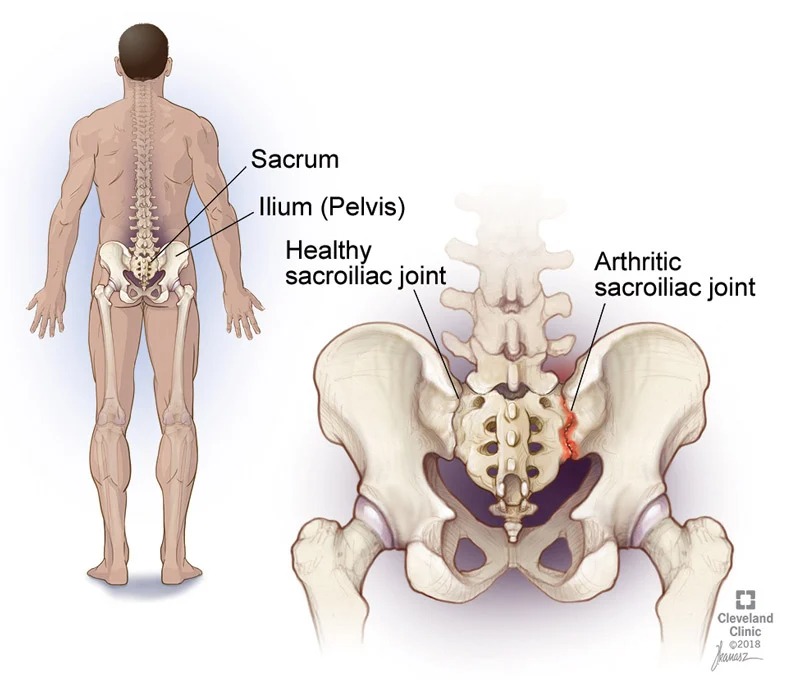
The characteristic x-ray change in AS is called the bamboo spine (seen at the top of this page), but this is usually seen only seen late in the disease. Inflammation of the sacroiliac joints, a common place of involvement in AS, can be seen on x-rays and is called sacroiliitis. However, when symptoms are first starting, the x-rays may be normal, and an MRI may be necessary to identify inflammation in the spine.
Treatment
The major aims of AS treatment include pharmacologic relief of pain and stiffness, as well as a physical therapy and lifestyle modification program aimed at preserving spinal mobility and preventing spinal deformity and disability. Prompt recognition and management of AS is essential to minimize the risk of further joint damage, disability, chronic pain, and other complications.
Formal instruction in proper posture and exercises emphasizing spinal mobility and strengthening of muscles is important. Range of motion exercises for the neck, shoulders and hips as well as deep-breathing exercises to maintain chest expansion should be performed by the patient daily. Of all therapeutic modalities, only regular exercise has been shown to curtail progression of spinal stiffness and restriction.
Treatments with non-steroidal anti-inflammatory medications (ex. Ibuprofen, naproxen) may reduce spinal stiffness and pain in many patients. However, for more severe cases, stronger therapies can be instituted that work to suppress your immune system to decrease inflammation.




