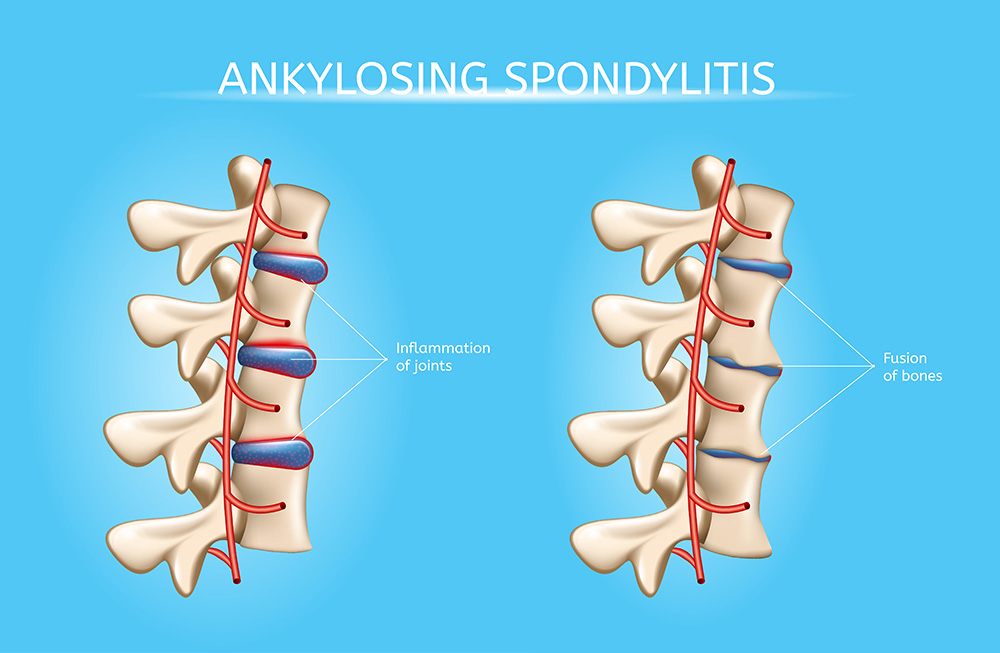
Ankylosing spondylitis is an inflammatory condition that, over time, can lead to the fusion of bones in the spine (vertebrae). This blending of the spine decreases its flexibility and causes a hunched-over posture. In severe cases, the ribs can be affected making it difficult to breathe deeply.
Symptoms of Ankylosing Spondylitis
Symptoms and signs typically appear during the early stages of adulthood. Other parts of the body can also become inflamed, the most common locations are the eyes. Early symptoms and signs of ankylosing spondylitis include pain and stiffness in the lower back and hips, particularly in the morning and after periods of inactivity. Other common symptoms include neck pain and fatigue. Over time, the symptoms might increase, decrease or remain constant at irregular intervals.
The areas most commonly affected are:
- The joint between the base of the spine and the pelvis
- The vertebrae in the lower back
- Areas where tendons and ligaments attach to bones, mainly in the spine, but sometimes along the back of the heel
- The cartilage between the breastbone and the ribs
- Hip and shoulder joints
When to see a doctor
Go to the doctor if you have low back or buttock pain that began slowly, was worse in the morning or woke you up from your sleep during the second half of the night. Particularly, ankylosing spondylitis may cause increased pain after exercise and decreased pain with rest.
Separately, it is advised to visit an eye doctor immediately if you have a painful red eye, severe light sensitivity, or blurred vision.
Causes
There is no specific known cause of ankylosing spondylitis, however, genetic factors seem to be involved. Specifically, individuals with the HLA-B27 gene are at a high likelihood of developing ankylosing spondylitis. However, only a few people with the gene have the condition.
Typically, the onset occurs during late adolescence or early adulthood. Males appear to be more adversely affected than females. The age at which the disease begins varies from adolescence to age 25, and the peak incidence is around 28 years old. Approximately 15% of American and European adults have been diagnosed with a childhood-onset form of the disease.
Complications
In extreme ankylosing spondylitis, the body attempts to heal the injury by forming new bone. This new bone grows over time to close the gap between the vertebrae. Eventually all of the sections of the bone fuse. These areas of the spine become rigid and inflexible. Also, fusion can make the ribcage stiffer, decreasing the capacity of the lungs and their function.
Other complications might include:
- Eye inflammation (uveitis). One of the most common complications of ankylosing spondylitis is uveitis, which can cause severe, acute pain in the eyes, sensitivity to light, and blurred vision.
- Compression fractures. Some patients’ bones become weak early in the course of ankylosing spondylitis. Weakened vertebrae can distort, which increases the severity of a drooping posture. vertebral fractures can affect and possibly injure the spinal cord and nerves that pass through the spine.
- Heart problems. Ankylosing spondylitis can lead to issues with the aorta, which is the largest artery in the body. The aorta that is inflamed can expand to the point that it distorts the shape of the aortic valve in the heart, this negatively affects the function of the valve. The inflammation associated with ankylosing spondylitis increases the likelihood of other diseases in the heart.
Treating Ankylosing Spondylitis
There is no known cure for ankylosing spondylitis, but treatments can reduce the severity of symptoms and, possibly, prevent the disease from progressing. The primary objectives of management include the pharmacological treatment of pain and stiffness, as well as a physical therapy and lifestyle modification program that seeks to preserve mobility in the spine or, at a minimum, prevent spinal deformation and disability. Additionally, the recognition and treatment of articular and extra-articular complications must be immediate.
The formal introduction of proper posture and exercises that emphasize spinal mobility and the strengthening of muscles is vital. Range of motion exercises for the neck, shoulders, and hips as well as deep-breathing exercises to maintain chest expansion should be part of the patient’s daily regimen. All therapeutic approaches have demonstrated an ability to limit the progression of spinal rigidity and immobility, only exercise has demonstrated this ability specifically.
Medications that don’t have a steroidal component can decrease spinal rigidity. For the most severe cases, more aggressive therapies can be employed.
Pacific Arthritis is a group of rheumatology experts in Los Angeles and Santa Monica who have undergone specialized training in the diagnosis and treatment of inflammatory diseases. Our experienced team is dedicated to providing immediate and long-lasting relief for your pain and symptoms. If you or a loved one is experiencing symptoms of Ankylosing Spondylitis, call (310) 297-9221 to schedule an appointment.